A new shock classification scheme released by the Society for Cardiovascular Angiography and Interventions (SCAI) and endorsed by the American College of Cardiology (ACC), American Heart Association, the Society of Critical Care Medicine and the Society of Thoracic Surgeons was recently applied in a retrospective study analyzing patients in the cardiac intensive care unit (CICU) at the Mayo Clinic. The study was published today in early view in the Journal of the American College of Cardiology (JACC).
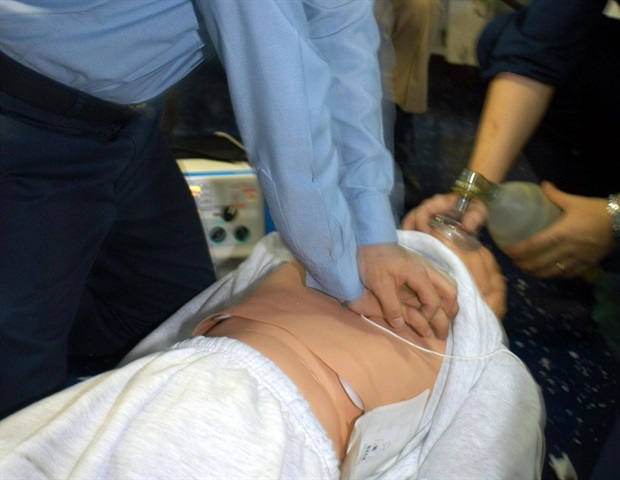
Cardiogenic shock (CS) is a condition in which the heart, often abruptly, cannot pump enough blood to meet the body's needs (Mayo Clinic). Most often accompanying larger heart attacks such as myocardial infarction (MI), outcomes for patients with cardiogenic shock complicating MI have not significantly improved over the last 30 years despite the development of various percutaneous mechanical circulatory support technologies and the national standard of emergent angioplasty and stenting. CS continues to be associated with high rates of morbidity and mortality, posing a therapeutic challenge for clinicians.
In the CICU we see a wide spectrum of shock severity including undifferentiated and mixed shock states, so we wanted to see whether a simplified, functional definition of the SCAI shock stages classification could be applied in an unselected CICU population using data from early after CICU admission. We found a dramatic incremental increase in mortality with each successive SCAI shock stage, with an additive mortality hazard among patients who suffered a cardiac arrest highlighting the importance of shock and cardiac arrest as major drivers of mortality in CICU patients. This confirms the validity of the SCAI CS stages construct and emphasizes its potential utility for clinical practice and future research."
Jacob C. Jentzer, MD, director for CICU Research at the Mayo Clinic in Rochester, MN
The study analyzed 10,004 patients admitted to the CICU between 2007 and 2015. The patients were classified as SCAI CS stages A through E, based on the presence of hypotension/tachycardia, hypoperfusion, deterioration and refractory shock.
Among the patients, 43 percent had acute coronary syndrome, 46 percent had heart failure and 12 percent had cardiac arrest. Study investigators found a stepwise increase in unadjusted CICU and hospital mortality with each increase in the SCAI shock stage. These results preliminarily validate the feasibility and prognostic value of the SCAI classification system.
"When we initially set out to create a new lexicon for cardiogenic shock, the goal was always to prove first and foremost that the increasing severity of shock predicted by the new classification would correspond to actual increasing hazard. This study is the first to validate the SCAI shock stages and add a relative risk to each successive stage, indicating in essence at what stage clinicians really have to worry about excessive mortality," said Srihari S. Naidu, MD, FSCAI, chair of the SCAI Shock expert consensus document writing group.
"The tremendous value of the SCAI CS staging system lies in its simplicity. It can easily be used across the spectrum of care from pre-hospital to intensive care unit and will allow clinicians to estimate mortality risk over time. When the SCAI Shock stage increases, it will be a signal to decide if transfer is warranted and potentially improve outcomes for patients. In addition, the SCAI CS classification highlights the potent risk of cardiac arrest and its effect on outcomes", said David Baran, MD, system director for Advanced Heart Failure, Transplant and MCS at Sentara Heart Hospital in Norfolk, Virginia.
Investigators believe the next step is prospective validation and implementation in clinical and research settings to ensure consistent outcomes reporting and to assess whether the effects of the tested intervention vary by CS stage.
Society for Cardiovascular Angiography and Interventions






No comments
Post a Comment