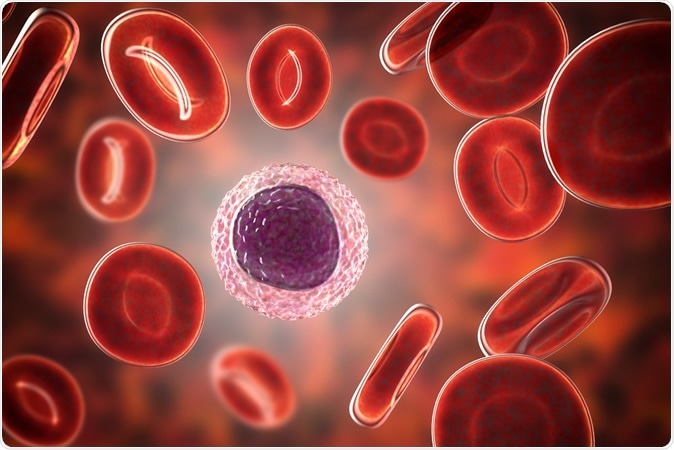
Lymphocyte surrounded by red blood cells, 3D illustration
In the current study, researchers found a positive and negative correlation with a host of blood molecules, including the ratio of neutrophils to lymphocytes, platelets to lymphocytes and monocytes to lymphocytes. Some of these were able to predict a good or bad outcome, while others were limited to only childhood tumors.
It would be useful to tell how far treatment would benefit the patient before embarking on these costly and potentially toxic therapies. The present study aims to explore the possibility of using biomarkers to predict the prognosis in MB.
The biomarkers they used included those associated with a poor outcome in solid tumors, like preoperative:
- neutrophil-to-lymphocyte ratio (NLR)
- platelet-to-lymphocyte ratio (PLR)
- monocyte-to-lymphocyte ratio (MLR)
- mean platelet volume (MPV)
- platelet distribution width (PDW)
- AGR (albumin-to-globulin ratio) w
How was the study done?
The study included 144 patients with MB, with the following break-up: 30 SHH, 25 WNT, 51 Group 3, and 38 Group 4 MB patients. 80% of these were children. 65% of patients were male. 76% had midline tumors while the rest were one-sided. All tumors were resected, with total resection being done in 53%. 80% received postoperative radiotherapy, while 55% received chemotherapy after surgery.The results
However, after adjusting for different subgroups, the most important prognostic biomarkers were NLR and PLR in childhood but not adult MB.Individually, a high NLR preoperatively predicted a poor prognosis in Group 3, while a high NLR and PLR indicated a poor outcome in Group 4 MB. WNT MB is known to be associated with a better survival chance than Group 3 MB, and this agrees with the lower NLR in this group.
Other factors like MLR and PDW showed no value in predicting the prognosis.
Why do these matter?
The researchers speculate that an increased number of neutrophils could enhance the invasion and metastasis of the MB because of the increased oxidative damage, which could damage DNA and increase the chances of mutations. Simultaneously, neutrophils release cytokines like interleukin-1 (IL-1), tumor necrosis factor (TNF) and vascular endothelial growth factor (VEGF), which promote tumor growth and spread.However, the presence of tumor infiltrating lymphocytes (TILs) was thought to be a sign of anti-tumor immunity, and a reduced TIL number meant a worse prognosis. When the NLR was high, therefore, it could be a sign of reduced TILs, and this could explain the poorer prognosis.
Platelet receptors play a role in encouraging tumor metastasis, and the growth of blood vessels to supply the tumor’s need for nutrition. Platelet activation also promotes inflammation which provides an ideal microenvironment for tumor growth, by causing high neutrophil and platelet counts, and low lymphocyte count.
While the study has limitations, its findings indicate that the preoperative PLR and NLR could be used to predict the prognosis in Group 3 and Group 4 MB.
The study is published in the journal Scientific Reports.
Journal reference:
Preoperative neutrophil to lymphocyte ratio and platelet to lymphocyte ratio are associated with the prognosis of group 3 and group 4 medulloblastoma. Ke Li, Wen-chao Duan, Hai-biao Zhao, Li Wang, Wei-wei Wang, Yun-bo Zhan, Tao Sun, Feng-jiang Zhang, Bin Yu, Ya-hui Bai, Yan-min Wang, Yu-chen Ji, Jin-qiao Zhou, Xian-zhi Liu, Zhi-feng Zhang & Zhen-yu Zhang. Scientific Reports, volume 9, Article number: 13239 (2019). https://doi.org/10.1038/s41598-019-49733-6. https://www.nature.com/articles/s41598-019-49733-6#Abs1






No comments
Post a Comment