In search of a possible cure for Alzheimer’s disease (AD), scientists have found out the molecular structure of a type of protein called beta amyloid that accumulates within brain cells, eventually killing them. This could help understand how to prevent these abnormal proteins from forming, leading to a cure or treatment for this killer disease.
AD is a progressive disorder afflicting over 5 million Americans. It inflicts a heavy cost on the victim and the caregiver, as it slowly sucks away memory, thinking, and judgment, leaving behind a vacuum in personality. No cure is currently known.
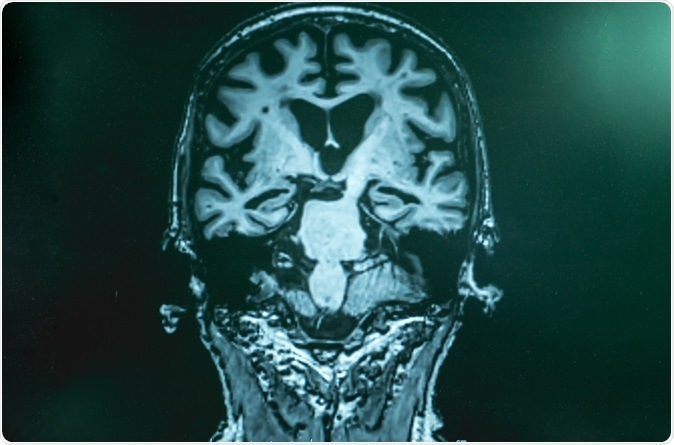
The brains of AD patients contain characteristic tangles and plaques caused by the accumulation of two types of abnormal proteins, namely, tau and beta amyloid respectively. There is no consensus as to how these are formed, or their actual role in the disease process. However, they are ubiquitous in this patient group.
The beta amyloid protein is actually a fragment of protein, and these bits join to form chains called fibrils. This fragment is abnormal because of misfolding at certain sites. In about 10% of cases this occurs for genetic reasons. However, in the vast majority, the natural amyloid protein undergoes misfolding.
Proteins are formed of amino acids in a specific sequence, depending on the protein involved. They then undergo various modifications, which ultimately affect their function. One type of modification is the post-translational modification, of which many examples are known to exist in beta-amyloid. These post-translational modifications are important in many ways.
In AD, post-translational modifications can in some cases increase the toxic effects of beta amyloid on the nerve cell. In other situations, they increase the rate of formation of neurofibrils above the normal. A third effect that has been observed is increased fibrillary strength.
However, there is not much knowledge as to the correlation between the type of modification and the resulting effect on the disease process. This was one area addressed by the present study, which aimed to find out the molecular build of one type of the beta amyloid protein and the physical and chemical attributes of the resulting fibril.
The team used high-resolution solid-state nuclear magnetic resonance spectroscopy to examine the structure of these altered protein fibrils. They described the complete molecular structure of one variant found to cause human AD, and also demonstrated that this structure could result in the spread of these protein fibrils to other parts of the brain at a greater speed.
The researchers looked at one chain comprised of 40 amino acid residues, called the Ser-8-phosphorylated Aβ40 (pS8-Aβ40) chain. They were able to demonstrate the presence of structural differences at various sites compared to all other known beta amyloid40 fibrils at its N-terminal end. The changes they observed were the presence of strong chemical interactions within the protein fibril that resulted in a close folding of the N-terminal end towards the amyloid core.
Moreover, their tests showed that this pathological variant was able to seed more wild-type monomers of beta-amyloid40 that occur in nature. The cross-seeded amyloid fibrils were also stronger, with a better core rigidity and resistance to heat, than the fibrils formed by the native or wild-type fibrils themselves. Thus these fibrils might replace wild-type beta amyloid because of their superior seeding capability and strength.
The scientists are already working on other variants of beta-amyloid fibrils. They are most interested in the way the differences in structure affect the ability of the fibrils to induce the formation of new fibrils, and how the cell is affected thereby.
The paper, entitled “Molecular structure of an N-terminal phosphorylated β-amyloid fibril,” was published in the journal Proceedings of the National Academy of Sciences on May 16, 2019.
Researcher Wei Qiang says, “We need to understand the molecular basis of the disease pathology. In doing so, we might one day create drugs that prevent the degenerative effects of the disease.”
Molecular structure of an N-terminal phosphorylated β-amyloid fibril, Zhi-Wen Hu, Liliya Vugmeyster, Dan Fai Au, Dmitry Ostrovsky, Yan Sun, Wei Qiang, Proceedings of the National Academy of Sciences Jun 2019, 116 (23) 11253-11258; DOI: 10.1073/pnas.1818530116, https://www.pnas.org/content/116/23/11253






No comments
Post a Comment